Connect With Us
Blog
Items filtered by date: March 2022
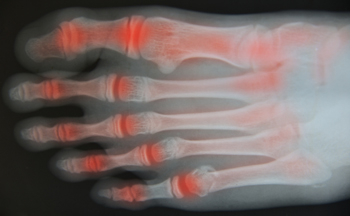
When Rheumatoid Arthritis Affects the Ankle
Rheumatoid arthritis (RA) is a progressive disease that causes the body’s immune system to mistakenly attack healthy tissue. RA can break down cartilage between bones in the ankle. Without healthy cartilage between ankle bones, bones rub together and cause friction that can lead to inflammation and pain in the ankle joint. In addition, RA can also weaken surrounding tissues that normally support and stabilize the ankle. Over time, the damage RA inflicts on the ankle can change how the joint functions and may lead to further destruction. A podiatrist can diagnose RA in your ankles and help determine the best course of treatment, which may include non-steroidal anti-inflammatory medications, corticosteroid injections, custom orthotics, physical therapy, and in some cases, surgery.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Tri-Town Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Arlington, Canton, and Chelsea, MA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Bunions and Bunionettes

Bunions are an acquired foot deformity where a misalignment in the bones of the big toe causes a protrusion to form on the outside of the foot at the toe’s joint. This forces the toe to angle toward the other toes rather than pointing straight ahead. Bunionettes, also known as tailor bunions, form on the outside of the pinky toe. Both bunions and bunionettes can cause pain, swelling, and soreness. Bunions that go untreated may lead to limited range of movement and will not get better on their own. Wearing proper footwear with lower heels, a rounded toe box and plenty of room for the toes can help you avoid getting a bunion or bunionette, although the shape of your feet, heredity, and certain medical conditions can also be contributing factors. If you have a bunion or bunionette, it's a good idea to seek the professional care of a podiatrist for treatment options.
If you are suffering from bunion pain, contact one of our podiatrists of Tri-Town Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Arlington, Canton, and Chelsea, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Get Professional Care for a Broken Foot or Ankle
Cracked Heels Can Cause More Than Cosmetic Issues
Cracked heels, or heel fissures, can develop when skin on the heel dries out and becomes callused. This dried out skin can then crack when weight placed on the heel causes the fat pad under the heel to spread out. If these cracks are left untreated, they can deepen to the point where they bleed or even become infected. This is not only painful, but can be very dangerous—especially for individuals with diabetes. Certain factors—along with having dry, thickened skin—can contribute to the formation of cracked heels, such as standing for prolonged periods of time, going barefoot, wearing open-backed shoes, and carrying extra weight. Also, diabetes, hypothyroidism, atopic dermatitis, psoriasis, and other conditions that can cause dry skin can be associated with cracked heels. Sometimes, cracked heels can be lessened by using topical water-retaining creams. If your cracked heels do not improve with regular moisturizing, if they are deep or bloody, or if you have diabetes, it is suggested that you seek professional treatment from a podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Tri-Town Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Arlington, Canton, and Chelsea, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
When Gout Flares up in the Big Toe Joint
If your big toe joint suddenly gets hot, red, swollen, and very painful, you could be having a gout flare. Gout is an arthritic condition that develops when excessive amounts of uric acid in the body cluster and crystallize on joints—most commonly the big toe joint. Symptoms from a gout flare can last for days or weeks and then completely disappear until the next flare occurs. You may be more at risk of developing gout if you have a family history of it, or if you are male, obese, drink alcohol, eat a lot of purine-rich red meat and seafood, or have certain health conditions like diabetes, kidney issues, hypertension, congestive heart failure, diabetes and more. If you believe you may have gout, it's a good idea to make an appointment with a podiatrist who can diagnose your condition through an exam and various tests, and help relieve your pain. In severe cases, where large deposits of gout form and normal pain relief methods do not provide relief (or there is joint dysfunction), surgery may be necessary.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Tri-Town Podiatry. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our offices located in Arlington, Canton, and Chelsea, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Do Plantar Warts Look Like?
Plantar warts are non-cancerous, rough growths that appear on pressure points located on the sole of the foot. They are caused by the human papillomavirus (HPV), which is spread through direct contact with a plantar wart or an object where HPV is present. Plantar warts are usually flat, and either brown, gray or flesh-colored. They can sometimes have black dots in the center, which are tiny capillaries that supply the wart with blood. Warts can grow individually or appear in clusters. They may be painful when you apply pressure to the bottom of the foot or walk on them. There are several types of therapies podiatrists can use to remove these warts permanently. If you notice a growth on the bottom of your foot that has the characteristics described here, please contact a podiatrist to confirm that what you see is a plantar wart and to receive proper care.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Tri-Town Podiatry. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Arlington, Canton, and Chelsea, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.